Your liver is one of the most vital and hardworking...

In the realm of medical innovation, few advancements have offered as much promise and potential as the pancreas transplant. This groundbreaking procedure has emerged as a beacon of hope for individuals grappling with the complexities of diabetes, particularly those facing the challenges of type 1 diabetes mellitus (T1DM) or severe cases of type 2 diabetes mellitus (T2DM). By replacing a malfunctioning pancreas with a healthy one, this surgical intervention has transformed the landscape of diabetes management, offering patients a chance at a life free from the shackles of constant glucose monitoring and insulin injections.
Understanding the Pancreas and Diabetes
The pancreas, a vital organ nestled behind the stomach, plays a pivotal role in regulating blood sugar levels and aiding in digestion. Within its intricate structure, specialized clusters of cells known as islets of Langerhans produce insulin, the hormone responsible for facilitating the uptake of glucose by cells for energy production. In individuals afflicted with diabetes, this delicate balance is disrupted, leading to aberrant blood sugar levels that can wreak havoc on various organ systems.
Type 1 diabetes, often diagnosed in childhood or adolescence, results from the autoimmune destruction of insulin-producing beta cells within the pancreas. Patients with T1DM rely on exogenous insulin administration to sustain life, meticulously monitoring their blood glucose levels and adjusting insulin doses accordingly. On the other hand, type 2 diabetes, typically associated with lifestyle factors such as obesity and sedentary behavior, entails insulin resistance, wherein cells fail to respond effectively to insulin signals.
The Promise of Pancreas Transplantation
Pancreas transplantation represents a beacon of hope for individuals ensnared by the relentless grip of diabetes. Unlike conventional insulin therapy, which merely manages symptoms without addressing the underlying pathology, this procedure offers the prospect of restoring normal glucose metabolism, liberating patients from the onerous burden of daily insulin injections and incessant glucose monitoring.
The Surgical Procedure
A pancreas transplant involves the meticulous surgical removal of a diseased or dysfunctional pancreas and its replacement with a healthy donor pancreas. This intricate procedure typically necessitates a team of highly skilled surgeons adept in abdominal organ transplantation. Depending on the patient’s specific medical needs and circumstances, pancreas transplantation may be performed in conjunction with kidney transplantation (simultaneous pancreas-kidney transplant, or SPK) for individuals with end-stage renal disease secondary to diabetes.
Types of Pancreas Transplants
- Simultaneous Pancreas-Kidney Transplant (SPK): This approach is reserved for individuals with both type 1 diabetes and end-stage renal disease requiring kidney transplantation. By replacing both organs simultaneously, SPK offers comprehensive restoration of metabolic function and renal function, affording recipients a newfound lease on life.
- Pancreas after Kidney Transplant (PAK): In cases where patients have previously undergone kidney transplantation and subsequently develop diabetes or experience deterioration in pancreatic function, a pancreas transplant may be performed following kidney transplantation.
- Pancreas Transplant Alone (PTA): This option is tailored for individuals with diabetes who do not require kidney transplantation but experience severe complications or glycemic instability despite optimal medical management. PTA aims to restore euglycemia and mitigate the risk of diabetes-related complications.
Benefits and Considerations:
Benefits
- Normalization of Blood Glucose Levels: Pancreas transplantation holds the promise of restoring physiological insulin secretion, thereby normalizing blood glucose levels and obviating the need for exogenous insulin therapy.
- Enhanced Quality of Life: Freed from the constraints of incessant glucose monitoring and insulin injections, recipients of pancreas transplants often report significant improvements in their quality of life, enjoying newfound freedom and independence.
- Prevention of Diabetes Complications: By restoring euglycemia and mitigating the risk of diabetes-related complications, pancreas transplantation offers a lifeline to individuals grappling with the debilitating consequences of uncontrolled diabetes.
Considerations
- Surgical Risks: Like any major surgical procedure, pancreas transplantation carries inherent risks, including bleeding, infection, graft rejection, and complications related to immunosuppressive therapy.
- Immunosuppression: To prevent rejection of the donor pancreas, recipients must undergo lifelong immunosuppressive therapy, which entails its own set of potential side effects and complications, including increased susceptibility to infections and metabolic disturbances.
- Donor Shortage: The success of pancreas transplantation hinges on the availability of suitable donor organs, and unfortunately, the supply often falls short of demand, necessitating judicious allocation and prioritization of candidates based on clinical urgency and compatibility.
Conclusion
In the ongoing battle against diabetes, pancreas transplantation stands as a beacon of hope, offering a transformative solution for individuals grappling with the relentless complexities of this debilitating disease. By restoring normal glucose metabolism and obviating the need for exogenous insulin therapy, this pioneering procedure has revolutionized the landscape of diabetes management, affording patients a newfound lease on life and the promise of a brighter, healthier future. However, as with any medical intervention, careful consideration of the risks and benefits is paramount, underscoring the importance of informed decision-making and comprehensive multidisciplinary care in maximizing patient outcomes.
Real Patients, Real Stories
Liver Transplant and Biliary Sciences Blogs
Understanding Alcoholic Fatty Liver Disease (AFLD)
By Dr. Manoj Shrivastav — Liver Specialist, Pune The liver...
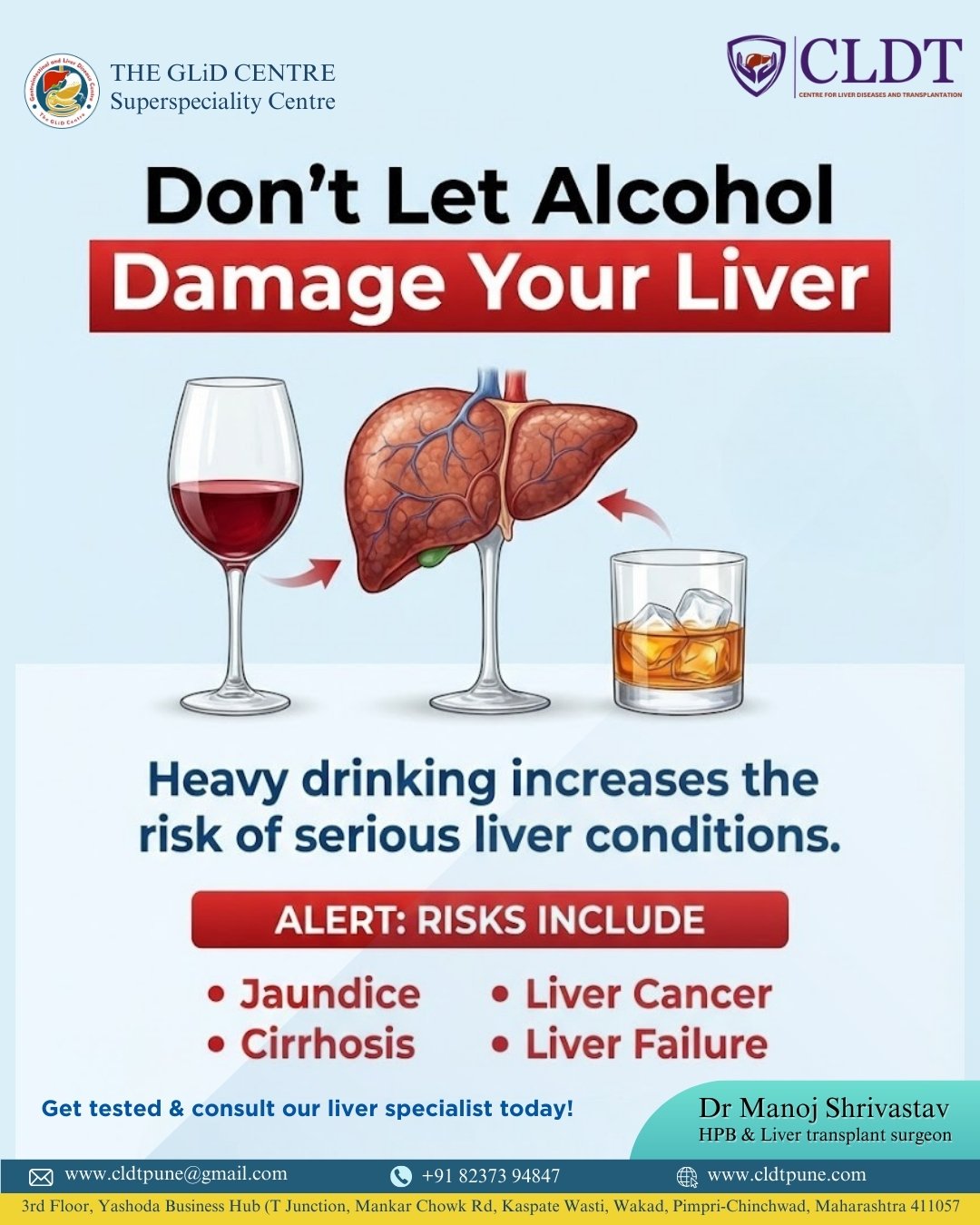
Liver Damage Due to Alcohol: Causes, Risks,
Alcohol consumption has become a common part of modern lifestyles....
Pune’s New Identity in Liver Transplantation :
यकृत प्रत्यारोपणातील पुण्याची नवी ओळख : डॉ. मनोज श्रीवास्तव यांचे...