Your liver is one of the most vital and hardworking...

Pancreatitis, whether acute or chronic, can be a debilitating condition marked by inflammation of the pancreas, a vital organ responsible for producing digestive enzymes and hormones like insulin. While many cases can be managed through medication and lifestyle changes, severe cases may require surgical intervention. In this article, we delve into the surgical options available for treating acute and chronic pancreatitis.
Acute Pancreatitis: Emergent Surgical Considerations
Acute pancreatitis typically presents suddenly and requires immediate medical attention. In mild cases, treatment may involve hospitalization for pain management, hydration, and fasting to allow the pancreas to heal. However, severe cases may necessitate surgical intervention to address complications such as infected pancreatic necrosis, pseudocysts, or obstruction of the bile duct or duodenum.
- Necrosectomy: In cases of infected pancreatic necrosis, where dead tissue becomes infected and leads to serious complications, a surgical procedure called necrosectomy may be necessary. This involves the removal of necrotic tissue from the pancreas to prevent further infection and promote healing. This procedure is often performed laparoscopically or through open surgery, depending on the severity and extent of the necrosis.
- Pseudocyst Drainage: Pseudocysts are fluid-filled sacs that can develop in the pancreas following an episode of acute pancreatitis. If these pseudocysts become large or symptomatic, they may require drainage through surgical or minimally invasive techniques. This can involve endoscopic drainage, where a flexible tube with a camera is inserted through the mouth into the stomach and small intestine to drain the pseudocyst, or surgical drainage if endoscopic methods are not feasible.
- Biliary or Duodenal Surgery: In cases where acute pancreatitis is caused by gallstones blocking the bile duct or by inflammation spreading to the duodenum, surgical intervention may be necessary to remove the obstruction. This can involve procedures such as cholecystectomy (removal of the gallbladder) or sphincterotomy (cutting of the sphincter muscle in the duodenum) to alleviate pressure on the pancreas and promote healing.
Chronic Pancreatitis: Long-Term Management through Surgery
Chronic pancreatitis is characterized by persistent inflammation of the pancreas, often leading to progressive damage and scarring of the pancreatic tissue. While initial treatment focuses on pain management, enzyme replacement therapy, and lifestyle modifications, surgery may be considered for patients with refractory symptoms or complications such as pancreatic duct strictures, pseudocysts, or pancreatic cancer.
- Pancreaticoduodenectomy (Whipple Procedure): In cases of chronic pancreatitis complicated by pancreatic cancer or severe pancreatic ductal strictures, a pancreaticoduodenectomy, commonly known as the Whipple procedure, may be recommended. This extensive surgery involves the removal of the head of the pancreas, part of the small intestine, gallbladder, and bile duct. It is a complex procedure associated with significant risks but can offer relief for patients with advanced pancreatic disease.
- Pancreatic Resection: For patients with localized disease or specific complications such as pseudocysts or pancreatic abscesses, surgical resection of the affected portion of the pancreas may be considered. This can involve removing the diseased portion of the pancreas while preserving healthy tissue to maintain pancreatic function as much as possible.
- Pancreatic Duct Procedures: In cases where chronic pancreatitis is complicated by strictures or blockages in the pancreatic ducts, surgical interventions such as pancreatic duct dilation, stenting, or surgical bypass procedures may be performed to restore pancreatic drainage and alleviate symptoms.
Conclusion
Surgery plays a crucial role in the management of both acute and chronic pancreatitis, addressing complications, alleviating symptoms, and improving quality of life for patients. However, surgical intervention should always be approached cautiously, with careful consideration of the risks and benefits, and tailored to the individual patient’s needs and circumstances. Close collaboration between patients, gastroenterologists, and surgical teams is essential to ensure optimal outcomes and long-term success in the management of pancreatitis.
Real Patients, Real Stories
Liver Transplant and Biliary Sciences Blogs
Understanding Alcoholic Fatty Liver Disease (AFLD)
By Dr. Manoj Shrivastav — Liver Specialist, Pune The liver...
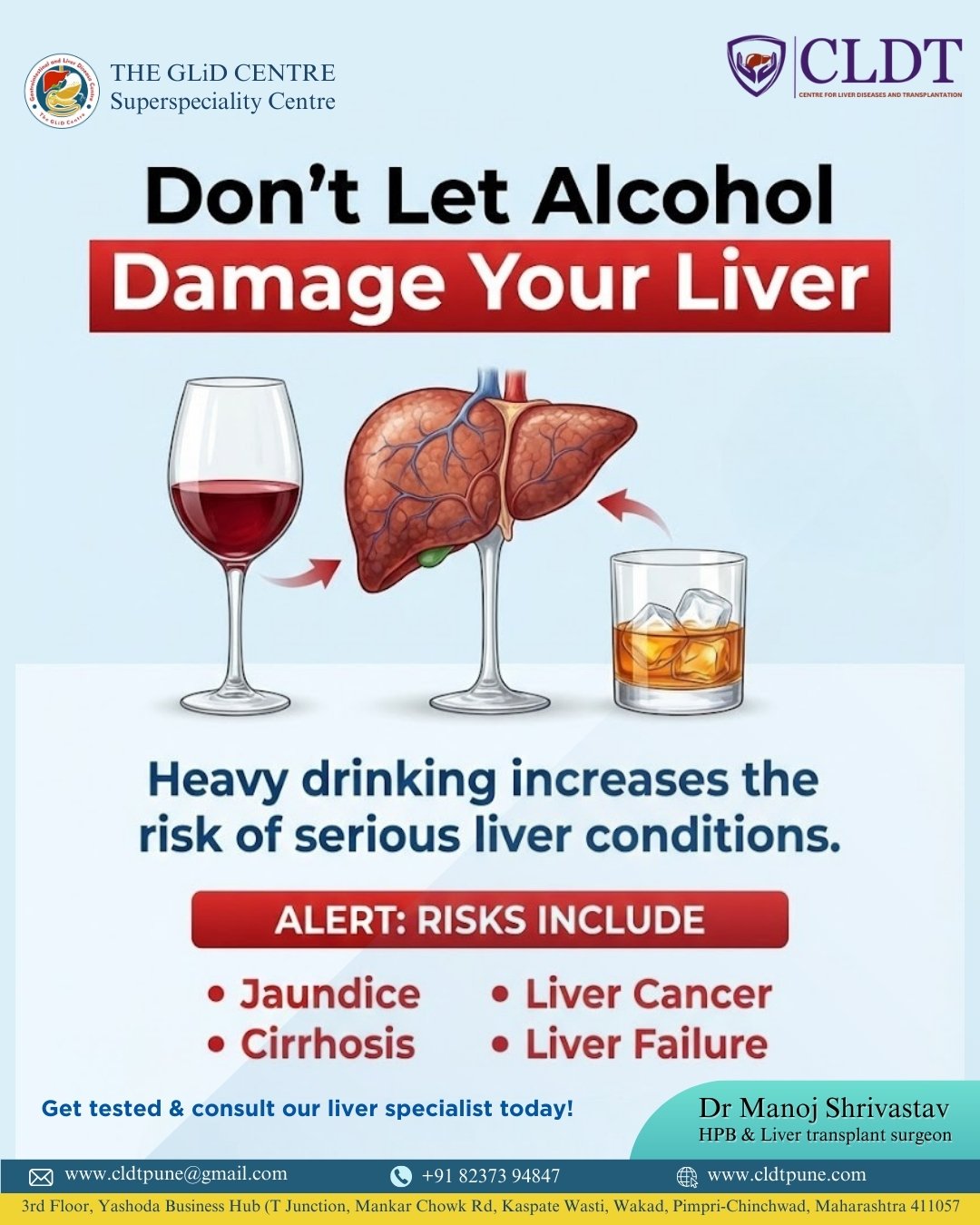
Liver Damage Due to Alcohol: Causes, Risks,
Alcohol consumption has become a common part of modern lifestyles....
Pune’s New Identity in Liver Transplantation :
यकृत प्रत्यारोपणातील पुण्याची नवी ओळख : डॉ. मनोज श्रीवास्तव यांचे...