Your liver is one of the most vital and hardworking...

Introduction:
Biliary atresia is a rare, life-threatening condition in infants where the bile ducts outside and inside the liver are scarred and blocked. Without treatment, bile remains in the liver, causing liver damage, cirrhosis, and eventually liver failure. This disorder is usually detected within the first few weeks to months of life. Effective management and treatment are crucial for improving the prognosis of affected infants.
Diagnosis and Early Detection
The early signs of biliary atresia include jaundice (yellowing of the skin and eyes), dark urine, pale stools, and hepatomegaly (an enlarged liver). Diagnosis typically involves a series of tests:
- Blood Tests: These check for elevated levels of bilirubin and liver enzymes.
- Imaging Tests: Ultrasound can reveal abnormalities in the liver and bile ducts. Hepatobiliary iminodiacetic acid (HIDA) scans help assess bile flow.
- Liver Biopsy: A biopsy can show changes in the liver that suggest biliary atresia.
- Operative Cholangiogram: This procedure involves injecting dye into the bile ducts to check for blockages or absence of ducts.
Early diagnosis is crucial because the success of treatment, particularly surgical intervention, is higher if performed early.
Kasai Procedure
The primary initial treatment for biliary atresia is the Kasai procedure (hepatoportoenterostomy), developed by Dr. Morio Kasai in 1959. This surgery aims to restore bile flow from the liver to the intestine by bypassing the blocked ducts. The key steps of the Kasai procedure include:
- Excision of Blocked Bile Ducts: The surgeon removes the atretic bile ducts outside the liver.
- Roux-en-Y Loop Creation: A segment of the small intestine is used to form a loop (Roux-en-Y loop), which is brought up to the liver.
- Anastomosis: The loop is connected to the liver at the site where the bile ducts exit (the porta hepatis).
Outcomes and Prognosis of Kasai Procedure
The success of the Kasai procedure is variable. If performed within the first two to three months of life, approximately 60-80% of infants may achieve some degree of bile drainage. However, even with successful bile flow, many children still face complications such as cholangitis (infection of the bile ducts), liver fibrosis, and portal hypertension.
Long-term prognosis after the Kasai procedure varies:
- Early Success: Infants who achieve good bile drainage may experience significant improvement and can avoid liver transplantation in the early years.
- Delayed Success or Failure: If bile flow is not adequately restored, liver damage continues, and these children typically require liver transplantation within the first few years of life.
Liver Transplantation
Liver transplantation is often the definitive treatment for biliary atresia, especially for those who do not respond to the Kasai procedure or who develop severe liver complications. Transplantation can be life-saving and offers a chance for a normal life expectancy.
- Indications for Transplantation: Indications include failed Kasai procedure, progressive liver failure, recurrent cholangitis, and complications such as intractable ascites or variceal bleeding.
- Donor Selection: Liver transplants can be from deceased donors or living donors (usually a parent or close relative). Living donor transplantation involves removing a portion of the donor’s liver.
- Surgical Procedure: The diseased liver is removed, and the donor liver or liver segment is transplanted. This complex surgery requires a multidisciplinary team.
Post-Transplant Care and Outcomes
Post-operative care is critical to the success of liver transplantation. This involves:
- Immunosuppression: Medications to prevent rejection of the transplanted liver.
- Monitoring: Regular follow-ups, blood tests, and imaging to monitor liver function and detect any complications.
- Managing Complications: Addressing issues such as infections, bile duct problems, and other post-surgical complications.
Outcomes for liver transplantation in biliary atresia have improved significantly over the years, with many children living into adulthood with good liver function and quality of life. However, lifelong medical care and monitoring are necessary.
Adjunct Therapies and Supportive Care
In addition to surgical interventions, supportive care plays a crucial role in managing biliary atresia:
- Nutritional Support: Many infants with biliary atresia have difficulty absorbing fat and fat-soluble vitamins (A, D, E, K). Specialized formulas and vitamin supplements are often necessary.
- Infection Prevention: Prophylactic antibiotics may be used to prevent cholangitis. Parents are also educated on signs of infection and when to seek medical help.
- Growth Monitoring: Regular monitoring of growth and development is essential, as chronic liver disease can affect overall growth.
Research and Future Directions
Ongoing research aims to improve outcomes for biliary atresia through:
- Early Detection: Developing non-invasive methods for earlier detection, such as blood biomarkers and advanced imaging techniques.
- Refinement of Surgical Techniques: Improving the Kasai procedure and transplantation techniques to enhance success rates and reduce complications.
- Regenerative Medicine: Exploring stem cell therapies and other regenerative approaches to repair liver damage and restore function.
Conclusion
Biliary atresia remains a challenging condition requiring prompt diagnosis and a multidisciplinary treatment approach. The Kasai procedure and liver transplantation are the mainstays of treatment, with supportive care playing a vital role in managing symptoms and complications. Advances in medical research hold promise for improving the long-term outcomes and quality of life for affected children. Early intervention and ongoing medical support are crucial for optimizing health and development in infants with biliary atresia.
Real Patients, Real Stories
Liver Transplant and Biliary Sciences Blogs
Understanding Alcoholic Fatty Liver Disease (AFLD)
By Dr. Manoj Shrivastav — Liver Specialist, Pune The liver...
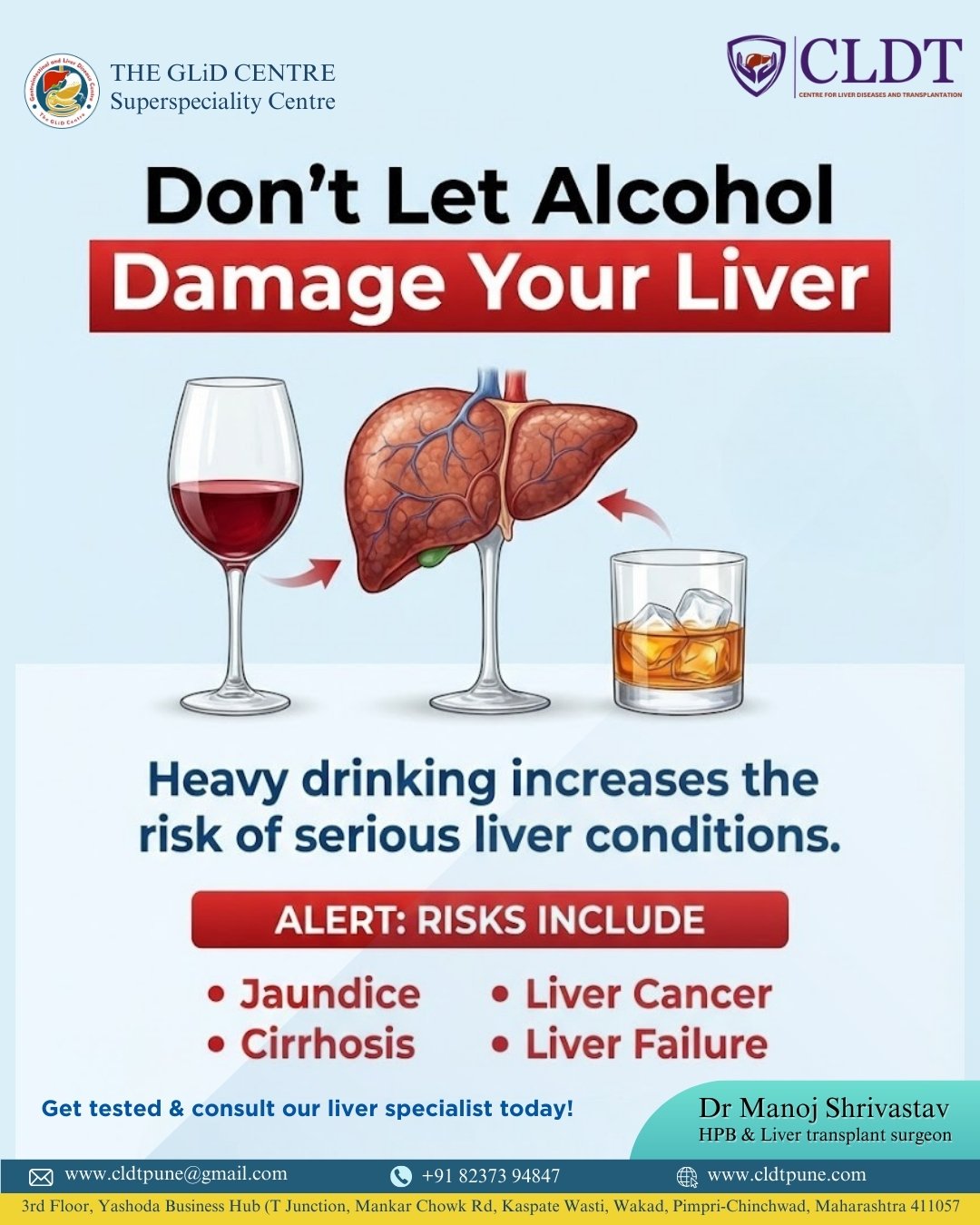
Liver Damage Due to Alcohol: Causes, Risks,
Alcohol consumption has become a common part of modern lifestyles....
Pune’s New Identity in Liver Transplantation :
यकृत प्रत्यारोपणातील पुण्याची नवी ओळख : डॉ. मनोज श्रीवास्तव यांचे...