Your liver is one of the most vital and hardworking...
Cholestatic liver diseases represent a diverse group of conditions characterized by impaired bile formation or flow, leading to the accumulation of bile acids and other substances within the liver. This results in cholestasis, a condition marked by jaundice, pruritus, and biochemical evidence of cholestasis (elevated alkaline phosphatase and bilirubin levels). Effective management of these diseases involves addressing the underlying cause, alleviating symptoms, and preventing complications.
Etiology and Classification
Cholestatic liver diseases can be broadly categorized into intrahepatic and extrahepatic causes. Intrahepatic cholestasis involves the bile ducts within the liver and can result from conditions such as primary biliary cholangitis (PBC), primary sclerosing cholangitis (PSC), drug-induced liver injury, and genetic disorders like Alagille syndrome. Extrahepatic cholestasis is due to obstruction in the bile ducts outside the liver, commonly caused by gallstones, strictures, or malignancies.
Diagnosis
Diagnosis begins with a thorough clinical evaluation, including history and physical examination. Key symptoms include jaundice, dark urine, pale stools, and pruritus. Blood tests reveal elevated levels of alkaline phosphatase, gamma-glutamyl transferase, and bilirubin. Imaging studies such as ultrasound, MRCP (magnetic resonance cholangiopancreatography), and ERCP (endoscopic retrograde cholangiopancreatography) are crucial for identifying the site and cause of obstruction.
Liver biopsy may be necessary in certain cases, especially for diagnosing intrahepatic cholestasis and assessing liver histology. Specific serological tests help diagnose autoimmune conditions like PBC (anti-mitochondrial antibodies) and PSC (ANCA).
General Management Principles
Management strategies for cholestatic liver diseases involve a combination of pharmacological treatments, surgical interventions, and supportive care:
1. Pharmacological Treatment
- Ursodeoxycholic Acid (UDCA): UDCA is a cornerstone treatment for PBC and PSC. It improves liver enzyme levels, delays disease progression, and enhances survival. The typical dose is 13-15 mg/kg/day.
- Obeticholic Acid: Used in PBC, especially in patients who do not respond adequately to UDCA. It activates farnesoid X receptor (FXR) to reduce bile acid synthesis.
- Cholestyramine: A bile acid sequestrant used to relieve pruritus. It binds bile acids in the intestine, reducing their reabsorption and systemic levels.
- Rifampin: An antibiotic that induces microsomal enzymes, enhancing bile acid metabolism and reducing pruritus.
- Antihistamines and Serotonin Receptor Antagonists: These are additional options for managing pruritus.
2. Nutritional Support
- Fat-Soluble Vitamins: Patients with cholestasis often have deficiencies in vitamins A, D, E, and K. Supplementation is crucial to prevent complications like osteoporosis, night blindness, and coagulopathy.
- Medium-Chain Triglycerides (MCTs): MCTs are easier to absorb than long-chain fats and are recommended in cases of fat malabsorption.
3. Liver Transplantation
- Indications: Liver transplantation is considered in patients with end-stage liver disease, severe pruritus unresponsive to medical treatment, or recurrent cholangitis. Both PBC and PSC are common indications for transplantation.
Disease-Specific Management Primary Biliary Cholangitis (PBC)
PBC is an autoimmune disease characterized by the destruction of small intrahepatic bile ducts. Management includes:
- UDCA: Standard therapy that slows disease progression.
- Obeticholic Acid: For patients with inadequate response to UDCA.
- Immunosuppressants: In refractory cases, drugs like methotrexate or mycophenolate mofetil may be considered.
Primary Sclerosing Cholangitis (PSC)
PSC involves inflammation and fibrosis of bile ducts, leading to strictures and cholestasis. Management focuses on:
- UDCA: Used in high doses, although its benefit is controversial.
- Endoscopic Interventions: ERCP with balloon dilatation or stenting to relieve strictures.
- Antibiotics: For treating bacterial cholangitis, a common complication.
- Liver Transplantation: Considered for advanced disease or recurrent cholangitis.
Drug-Induced Cholestasis
Cholestasis can result from various medications, including antibiotics, anabolic steroids, and oral contraceptives. Management involves:
- Discontinuation of the Offending Drug: Essential first step.
- Supportive Care: Monitoring liver function and managing symptoms until recovery.
Genetic and Pediatric Cholestasis
Conditions like Alagille syndrome and progressive familial intrahepatic cholestasis (PFIC) require a multidisciplinary approach:
- Medical Therapy: UDCA, fat-soluble vitamin supplementation, and nutritional support.
- Surgical Interventions: Procedures like biliary diversion may be necessary in PFIC.
- Liver Transplantation: Often required in advanced or refractory cases.
Complications and Their Management
Chronic cholestasis can lead to several complications requiring specific interventions:
1. Osteoporosis
- Vitamin D and Calcium Supplementation: Regular monitoring and supplementation to prevent bone loss.
- Bisphosphonates: Used in cases of confirmed osteoporosis.
2. Fat-Soluble Vitamin Deficiency
- Regular Monitoring and Supplementation: Essential to prevent complications like bleeding (vitamin K deficiency), vision problems (vitamin A deficiency), and neurological symptoms (vitamin E deficiency).
3. Cholangitis
- Antibiotic Therapy: Prompt treatment of infections.
- Endoscopic or Surgical Drainage: For obstructive cholangitis.
Conclusion
Management of cholestatic liver diseases requires a comprehensive and individualized approach. Early diagnosis and appropriate therapeutic interventions can significantly improve outcomes and quality of life for patients. Collaboration between hepatologists, gastroenterologists, surgeons, and nutritionists is crucial for optimal management of these complex conditions. Future research and advances in therapy hold promise for more effective treatments and better patient outcomes.
Real Patients, Real Stories
Liver Transplant and Biliary Sciences Blogs
Understanding Alcoholic Fatty Liver Disease (AFLD)
By Dr. Manoj Shrivastav — Liver Specialist, Pune The liver...
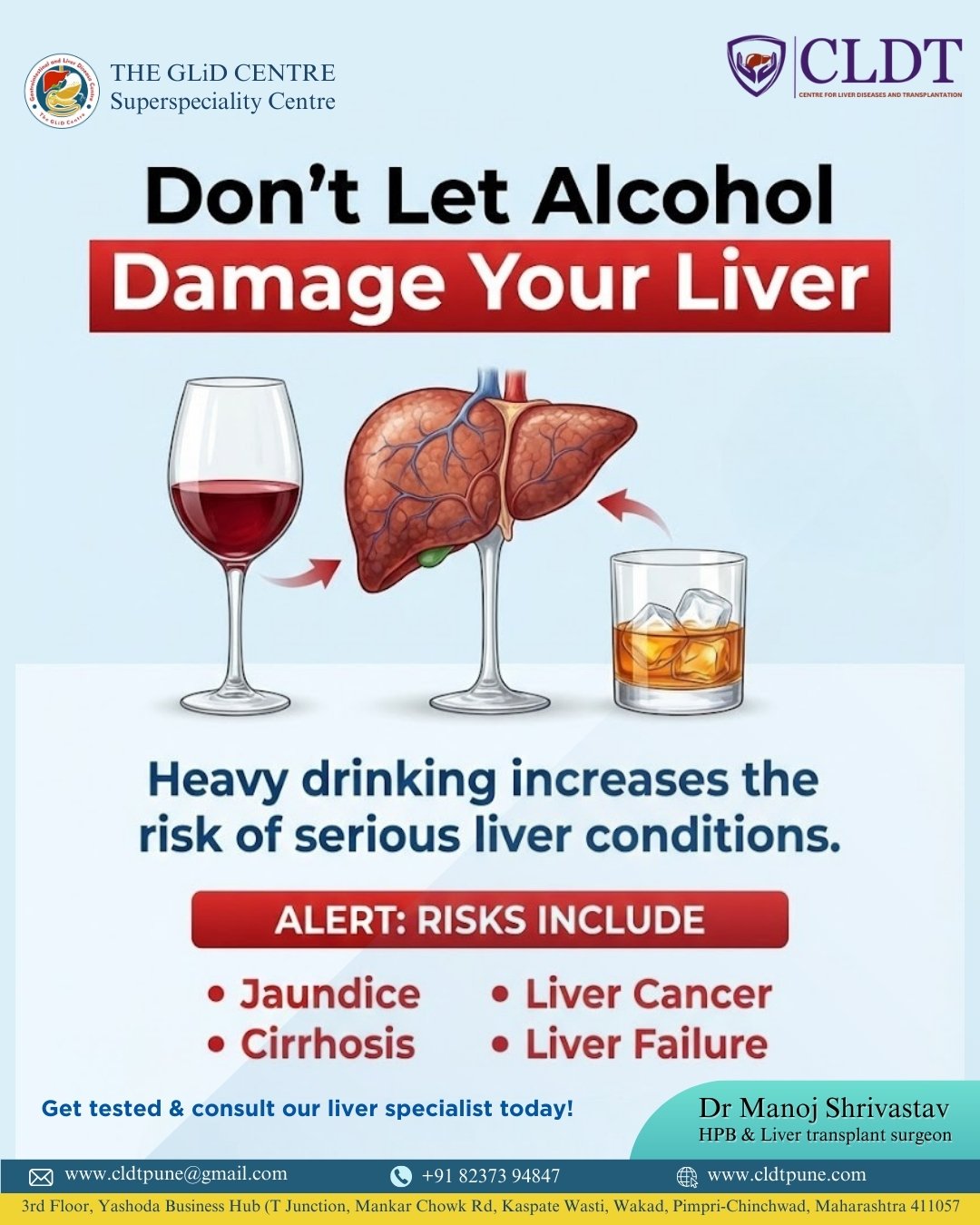
Liver Damage Due to Alcohol: Causes, Risks,
Alcohol consumption has become a common part of modern lifestyles....
Pune’s New Identity in Liver Transplantation :
यकृत प्रत्यारोपणातील पुण्याची नवी ओळख : डॉ. मनोज श्रीवास्तव यांचे...