Your liver is one of the most vital and hardworking...
Effective management of these conditions requires a multifaceted approach that integrates surgical, medical, and supportive care tailored to the individual patient’s needs.
Hepatocellular Carcinoma (HCC) Diagnosis and Staging
The management of HCC begins with accurate diagnosis and staging. Diagnostic modalities include imaging techniques such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI). Biopsy may be performed to confirm the diagnosis. Staging is typically done using the Barcelona Clinic Liver Cancer (BCLC) staging system, which helps guide treatment decisions.
Treatment Options
1.Surgical Resection
- Surgical resection remains the preferred treatment for patients with early-stage HCC and preserved liver function. The goal is to completely remove the tumor while preserving as much healthy liver tissue as possible. Patients with single tumors or small tumors (<5 cm) without vascular invasion are ideal candidates.
2.Liver Transplantation
- Liver transplantation offers a potentially curative option for patients with early-stage HCC (meeting the Milan criteria: single tumor ≤5 cm or up to three tumors ≤3 cm) and underlying liver cirrhosis. This approach addresses both the cancer and the underlying liver disease.
3.Ablative Therapies
- Radiofrequency Ablation (RFA): RFA is effective for small tumors (<3 cm) and involves the use of high-frequency electrical currents to destroy cancer cells.
- Microwave Ablation (MWA): Similar to RFA, MWA uses microwave energy to generate heat and ablate tumor tissues.
- Percutaneous Ethanol Injection (PEI): This method involves injecting ethanol directly into the tumor, leading to cell death. It is less commonly used today but can be effective for small lesions.
4.Transarterial Therapies
- Transarterial Chemoembolization (TACE): TACE involves delivering chemotherapy directly to the tumor through its blood supply and simultaneously blocking the artery to cut off the tumor’s blood supply. It is commonly used for intermediate-stage HCC.
- Transarterial Radioembolization (TARE): Also known as selective internal radiation therapy (SIRT), this method uses radioactive beads to deliver targeted radiation to the tumor via the hepatic artery.
5.Systemic Therapies
- Sorafenib and Lenvatinib: These tyrosine kinase inhibitors (TKIs) have been standard treatments for advanced HCC, showing benefits in prolonging survival.
- Immunotherapy: The introduction of immune checkpoint inhibitors, such as nivolumab and pembrolizumab, has opened new avenues in the treatment of advanced HCC. These drugs help the immune system recognize and attack cancer cells.
- Combination Therapies: Recent trials are exploring the efficacy of combining TKIs with immunotherapy, showing promising results in improving overall survival rates.
6.Radiation Therapy
- External beam radiation therapy (EBRT) and stereotactic body radiation therapy (SBRT) can be used for patients with unresectable tumors or those who are not candidates for other local therapies.
Hepatoblastoma Diagnosis and Staging
Hepatoblastoma, the most common liver cancer in children, is typically diagnosed in patients under the age of 5. The diagnosis involves imaging studies such as ultrasound, CT, and MRI, along with biopsy and serum alpha-fetoprotein (AFP) levels, which are usually elevated in hepatoblastoma. The PRETEXT (PRETreatment EXTent of disease) staging system is used to guide treatment.
Treatment Options
1.Surgical Resection
- Complete surgical resection is the cornerstone of hepatoblastoma treatment. For tumors that are initially resectable, surgery is performed upfront. For unresectable tumors, neoadjuvant chemotherapy is used to shrink the tumor to make surgery feasible.
2.Chemotherapy
- Preoperative (Neoadjuvant) Chemotherapy: Chemotherapy is often administered before surgery to reduce tumor size and facilitate complete resection. Commonly used agents include cisplatin, doxorubicin, vincristine, and cyclophosphamide.
- Postoperative (Adjuvant) Chemotherapy: After resection, adjuvant chemotherapy is given to eradicate microscopic residual disease and reduce the risk of recurrence.
3.Liver Transplantation
- For tumors that remain unresectable despite chemotherapy, liver transplantation is considered. This approach has shown success in achieving long-term survival in select patients.
4.Other Therapies
- Radiation Therapy: Although not commonly used, radiation therapy may be considered in cases of incomplete resection or for palliation of symptoms in metastatic disease.
- Targeted Therapy: Research into molecularly targeted therapies is ongoing, aiming to identify specific pathways involved in hepatoblastoma progression that can be therapeutically targeted.
Multidisciplinary Approach
Effective management of liver tumors requires a multidisciplinary team approach, involving hepatologists, oncologists, surgeons, radiologists, and pathologists. The treatment plan is individualized based on the tumor stage, liver function, patient age, and overall health status. Supportive care, including nutritional support, management of liver dysfunction, and psychosocial support, is also crucial for optimizing outcomes.
Follow-up and Surveillance
Post-treatment surveillance is vital for early detection of recurrence. Regular follow-up includes clinical assessments, imaging studies, and monitoring of tumor markers such as AFP levels. The frequency and duration of follow-up depend on the initial stage of the tumor and the type of treatment received.
Research and Future Directions
Ongoing research aims to improve the outcomes of liver cancer treatment through:
- Advancements in Surgical Techniques: Minimally invasive and robotic-assisted surgeries are being explored to reduce morbidity and enhance recovery.
- Novel Chemotherapeutic Agents: New drugs and combinations are being tested in clinical trials to find more effective and less toxic treatments.
- Personalized Medicine: Genetic and molecular profiling of tumors can help tailor therapies to individual patients, potentially improving efficacy and reducing side effects.
- Immunotherapy: Expanding the use of immunotherapy and understanding the mechanisms of resistance can lead to more effective treatment strategies.
- Targeted Therapy: Identification of novel molecular targets and development of targeted agents can provide new treatment options for patients with refractory or advanced disease.
Conclusion
The management of liver tumors, particularly HCC and hepatoblastoma, involves a combination of surgical, medical, and supportive therapies tailored to the patient’s specific condition. Advances in diagnostic techniques, surgical methods, chemotherapy, and emerging therapies like immunotherapy and targeted therapy hold promise for improving survival and quality of life for patients. A multidisciplinary approach and ongoing research are essential for continued progress in the treatment of these challenging cancers.
Real Patients, Real Stories
Liver Transplant and Biliary Sciences Blogs
Understanding Alcoholic Fatty Liver Disease (AFLD)
By Dr. Manoj Shrivastav — Liver Specialist, Pune The liver...
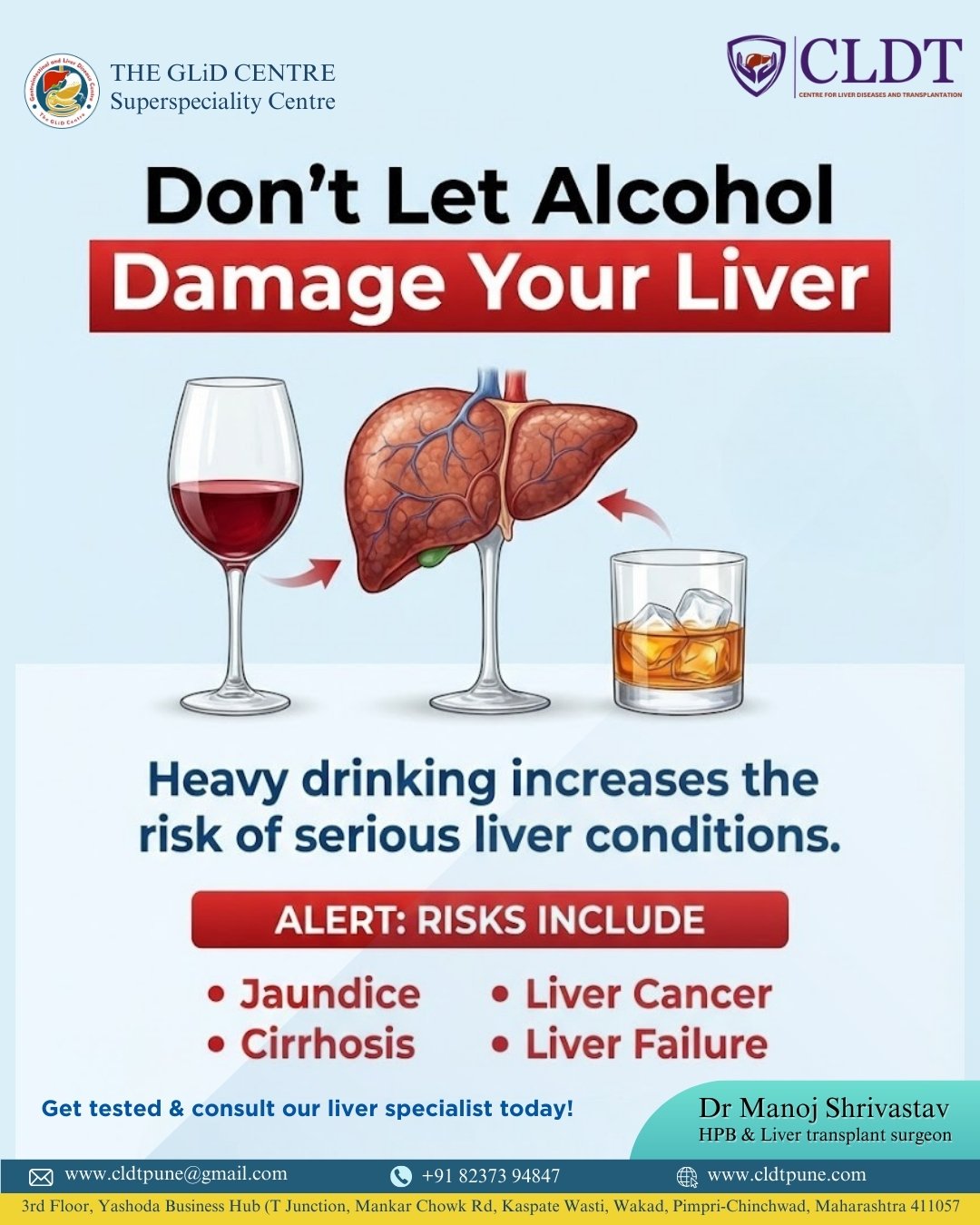
Liver Damage Due to Alcohol: Causes, Risks,
Alcohol consumption has become a common part of modern lifestyles....
Pune’s New Identity in Liver Transplantation :
यकृत प्रत्यारोपणातील पुण्याची नवी ओळख : डॉ. मनोज श्रीवास्तव यांचे...