Your liver is one of the most vital and hardworking...

Introduction
Portal hypertension is a significant medical condition characterized by increased pressure in the portal venous system, which can lead to serious complications, including variceal bleeding, ascites, and encephalopathy. In children, this condition presents unique challenges and requires specialized approaches for management. Two particular conditions that often cause portal hypertension in children are Extrahepatic Portal Venous Obstruction (EHPVO) and Non-Cirrhotic Portal Fibrosis (NCPF). This article delves into the management strategies for portal hypertension in pediatric patients, with a focus on EHPVO and NCPF.
Portal Hypertension in Children
Portal hypertension in children can result from various etiologies, including congenital anomalies, liver diseases, and vascular conditions. The management goals are to prevent and control complications, enhance quality of life, and address the underlying cause when possible. The treatment approach is multidisciplinary, involving hepatologists, gastroenterologists, radiologists, and surgeons.
Extrahepatic Portal Venous Obstruction (EHPVO)
EHPVO is a common cause of portal hypertension in children, characterized by the obstruction of the extrahepatic portal vein, leading to the development of portal collateral vessels and varices. This condition is often idiopathic but can result from neonatal umbilical vein catheterization, infections, or thrombophilia.
Diagnosis
The diagnosis of EHPVO involves a combination of clinical evaluation, imaging studies, and endoscopic procedures. Doppler ultrasound is the primary imaging modality, revealing the absence of flow in the portal vein and the presence of collateral circulation. Magnetic resonance angiography (MRA) and computed tomography angiography (CTA) can provide detailed vascular anatomy. Endoscopy is crucial for identifying esophageal and gastric varices.
Management
- Variceal Bleeding Prevention and Control:
- Endoscopic Therapy: Endoscopic variceal ligation (EVL) is preferred for the prevention and treatment of variceal bleeding. Sclerotherapy is an alternative when EVL is not feasible.
- Beta-Blockers: Non-selective beta-blockers, like propranolol, can reduce portal pressure and are sometimes used, although their role in children is less defined than in adults.
- Emergent Management of Bleeding: Acute variceal hemorrhage is managed with intravenous vasoactive drugs (e.g., octreotide), endoscopic hemostasis, and blood transfusions as needed.
- Surgical and Radiological Interventions:
- Shunt Surgery: Surgical creation of shunts (e.g., meso-Rex shunt) can restore portal venous flow to the liver, particularly in EHPVO. The meso-Rex bypass is the preferred option as it reestablishes physiological blood flow.
- Transjugular Intrahepatic Portosystemic Shunt (TIPS): TIPS is less commonly used in children but may be considered in refractory cases.
- Management of Associated Conditions:
- Splenomegaly and Hypersplenism: Symptomatic hypersplenism may necessitate splenectomy, although this is often avoided due to the risk of post-splenectomy sepsis.
- Growth and Nutritional Support: Regular monitoring and support for growth and nutrition are essential, as chronic portal hypertension can affect overall health and development.
Non-Cirrhotic Portal Fibrosis (NCPF)
NCPF, also known as idiopathic portal hypertension, is characterized by periportal fibrosis without significant liver cell injury. This condition is less common but poses distinct management challenges.
Diagnosis
NCPF is diagnosed based on clinical features, imaging, liver biopsy, and the exclusion of other causes of portal hypertension. Imaging studies may show splenomegaly and portal vein abnormalities without cirrhosis. Liver biopsy typically reveals periportal fibrosis with minimal inflammation or necrosis.
Management
- Control of Portal Hypertension:
- Pharmacological Therapy: Similar to EHPVO, beta-blockers may be used to reduce portal pressure, though evidence in pediatric NCPF is limited.
- Endoscopic Surveillance and Intervention: Regular endoscopic monitoring for varices is essential. Prophylactic EVL can be performed to prevent bleeding.
- Surgical Options:
- Shunt Surgery: In severe cases, portosystemic shunting may be considered to decompress the portal system.
- Liver Transplantation: Rarely, intractable symptoms or complications may necessitate liver transplantation, although this is uncommon for NCPF.
- General Supportive Care:
- Nutritional Support: Ensuring adequate nutrition and growth monitoring is vital. Nutritional deficiencies should be corrected.
- Management of Complications: Ascites and other complications are managed symptomatically, often with diuretics and dietary modifications.
Conclusion
The management of portal hypertension in children, particularly in conditions like EHPVO and NCPF, requires a comprehensive and tailored approach. Preventing and controlling variceal bleeding through endoscopic therapy and appropriate use of medications are critical components. Surgical interventions, including shunt surgeries, play a significant role in selected cases. Multidisciplinary care involving hepatologists, gastroenterologists, and surgeons is essential to optimize outcomes and improve the quality of life for affected children. Ongoing research and clinical trials are necessary to refine these management strategies and develop new treatments for pediatric portal hypertension.
Real Patients, Real Stories
Liver Transplant and Biliary Sciences Blogs
Understanding Alcoholic Fatty Liver Disease (AFLD)
By Dr. Manoj Shrivastav — Liver Specialist, Pune The liver...
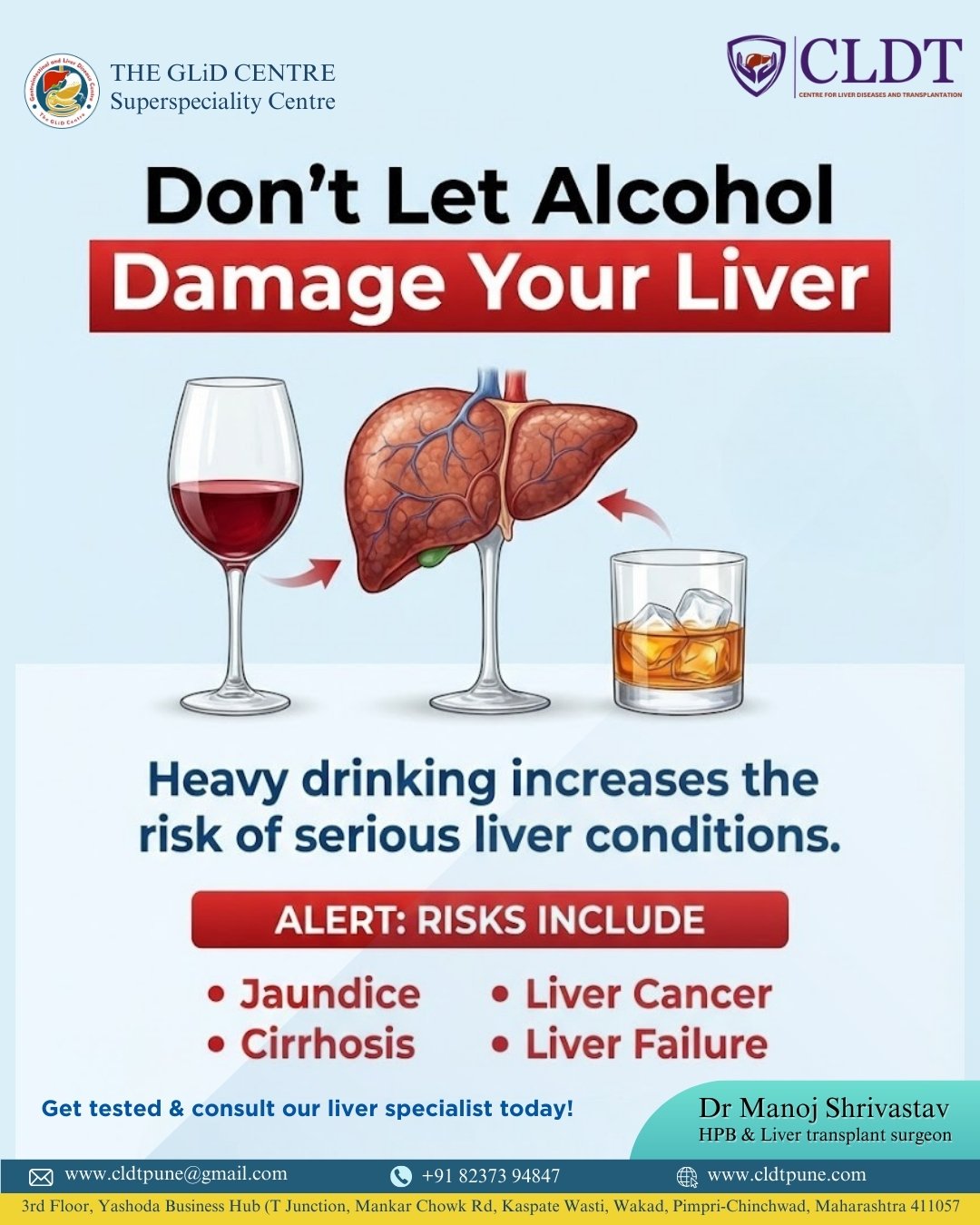
Liver Damage Due to Alcohol: Causes, Risks,
Alcohol consumption has become a common part of modern lifestyles....
Pune’s New Identity in Liver Transplantation :
यकृत प्रत्यारोपणातील पुण्याची नवी ओळख : डॉ. मनोज श्रीवास्तव यांचे...